This article provides succinct insights on fentanyl, as a medicine, a new drug related to online drug markets, and a reason to invest more (not less) in community-led harm reduction initiatives.
A brief history of the medical application of fentanyl:
Every drug in society, regardless of classification and purpose, has a history often rooted in the realms of medicine, whether ancient or modern, with each drug subject to the moral and ethical fibres of society acting to shape how the drug will be perceived and what connotations will be attached to its usage (Gossop 2013).
Fentanyl belongs to a depressant class of drugs known as opioids, a term that has expanded from its original denotation of drugs derived from the opium poppy, to include synthetic narcotics that have opiate-like activities but are not derived from opium (Mosby 2013). This places fentanyl in the same class of drugs as morphine, codeine, and heroin. However, unlike heroin, it carries a prescription drug status, despite being 50 times more potent than heroin and 100 times more potent than morphine (Stanley 2005).
Fentanyl was developed in the 1950s by Paul Janssen, founder of Janssen Pharmaceuticals (a division of Johnson & Johnson). Janssen’s experimentations in altering the basic structure of meperidine to increase the lipid solubility resulted in the discovery of increasingly potent molecular entities with synthetic opioid analgesics to be tested in animal models, the best of which was termed fentanyl (Stanley 2005). Janssen’s discovery initially impressed anaesthetists due to the rapid onset in which fentanyl crosses the blood-brain barrier. Most notably, George De Castro’s praise for fentanyl led to its approval for use during surgical procedures in Europe in the early to mid-1960s (Stanley 2005).
Wider acceptance of fentanyl in North America took more consideration, as the U.S. Food and Drug Administration (FDA), in partnership with Robert Dripps, Chairman of Anaesthesiology at the University of Pennsylvania, expressed dire concern over the high potential for abuse and the medical necessity of a drug 100 times more potent than morphine (Stanley 2005).
FDA approval came in 1968 in the form of a mixture of fentanyl and droperidol called Innovar, on the rationale that the negative psychological impacts of droperidol would factor out any real likelihood of recreational abuse. Innovar introduced the ‘neurolept anaesthetic technique’ to Europe, however, it never caught on or became widely accepted in the USA, which lead to a gradual reversion to fentanyl as a sole anaesthetic agent, with FDA approval given in 1972 (Stanley 2005).
At present in Australia, fentanyl is used for major trauma and surgery, as well as a pharmaceutical opioid for the treatment of chronic cancer pain, primarily administered via slow-release patches.
Fentanyl and the dark web
The Internet and digital technology have given rise to cryptocurrencies, the capacity for online anonymity and surveillance, and ‘hidden’ or end-to-end encrypted web portals commonly known as ‘the dark web’. In this context, more than 1000 illicit and new psychoactive substances (NPS) have been recorded being bought and sold on the dark web, including fentanyl.
Research from Quintana et al. revealed through drug analysis of heroin purchased from various drug crypto markets on the dark web that fentanyl is used as an adulterant, as well as fentanyl derivatives, like ocfentanil, butyrfentanyl and acetylfentanyl, (Quintana et al. 2016). Fentanyl derivatives have existed since the 1970s as synthetic designer drugs or NPS (Ritter et al. 2017). Most of these derivatives, such as ocfentanil, are non-controlled substances with high-risk profiles, especially when sold as or assumed to be heroin (Quintana et al. 2016). As well as being an adulterant, fentanyl is also advertised and sought after in online markets as a high strength opioid.
Cryptocurrency drug markets have existed since the early 2000s, the most infamous of which was Silk Road, which was shut down by the FBI in 2013. But at that point in time, more than 30 other online platforms already existed and Silk road resurfaced soon after the blitz too, indicating the high degree of resilience to disruptions. The advent of the Internet and related ICT has influenced drug trends and caused changes in availability, but this should not be assumed to mean that the illicit market has grown or become more dangerous because of technological advances. Rather, the emphasis on criminalising drug use, combined with an under-investment in health, particularly community-led health promotion and harm reduction initiatives, has always and continues to make drug use more high risk, and makes delivering effective health promotion and harm reduction services more difficult.
Fentanyl and harm reduction
Fentanyl is available from several sources, in the recreational drug market it is commonly manufactured from clandestine sources mixed into heroin, cocaine, oxycodone, hydrocodone, or alprazolam (Xanax) containing tablets (Kuczyńska et al. 2018). As prescription fentanyl is primarily administered in the form of transdermal patches, the drug can also be extracted from these patches to be injected, though the patches can also be swallowed (Kuczyńska et al. 2018).
The use of pharmaceuticals in Australia is a growing public health concern and is responsible for a far greater rate of drug-related harm including death than all illicit drugs combined (AIHW 2018). Aging Australians are most at risk of pharmaceutical drug-related harm, with painkillers and opioids being most commonly involved in adverse events (AIHW 2016). Fentanyl has been listed on Australia’s Pharmaceutical Benefits Scheme (PBS) since 2006, however, prior to 2012, presentations among PWID to inject fentanyl in Australia’s medically supervised injecting centre in Kings Cross, Sydney, were rare and sporadic (Latimer et al. 2016). Fentanyl overdoses have been increasing (shown in figure 5) and fentanyl-related mortality in Australia has shown that approximately half of the deaths involved polydrug toxicity. 2018 data from the Illicit Drug Reporting System (IDRS) revealed that among people who inject drugs (PWID), pharmaceuticals are often substituted, with non-prescribed fentanyl use reported at 7% among PWID, with morphine and oxycodone being the most abused of pharmaceuticals (IDRS cited in AIHW 2018).
The National Drug and Alcohol Research Centre (NDARC) reported 163 fentanyl-related deaths during 2000-2011 with the primary age group affected being over 47 years. Prescription fentanyl use is most prevalent in Australians aged over 80 years (NDARC cited in Roxburgh et al. 2013). This presents unique challenges in how to address risk factors among an ageing population whose need for pain management medicine is a contributing factor.
Although mortality related to fentanyl in Australia is low, it has made an impact. For example, there was a cluster of fentanyl-laced heroin deaths in Melbourne in 2015 (Rodda et al. 2017), an acetyl-fentanyl death in Western Australia in 2017 (Moss et al. 2017), and 60 Minutes produced a feature in 2018 on a Gold Coast teenager who died from an accidental fentanyl overdose after being prescribed it for back pain while playing gridiron in the USA. His family called for the prescription drug to be banned.
Several alerts and warnings have been issued in Australia regarding fentanyl. In October 2020 and on 28 January 2021, respectively, NSW Health issued drug warnings: ‘Cocaine and ketamine may contain the dangerous opioids fentanyl and acetylfentanyl’ (see https://www.health.nsw.gov.au/aod/public-drug-alerts/Pages/cocaine-or-ketamine-contains-fentanyl.aspx); and ‘Heroin may contain fentanyl and acetylfentanyl, which are dangerous opioids’ (see https://www.health.nsw.gov.au/aod/public-drug-alerts/Pages/heroin-may-contain-fentanyl-sydney-update.aspx)
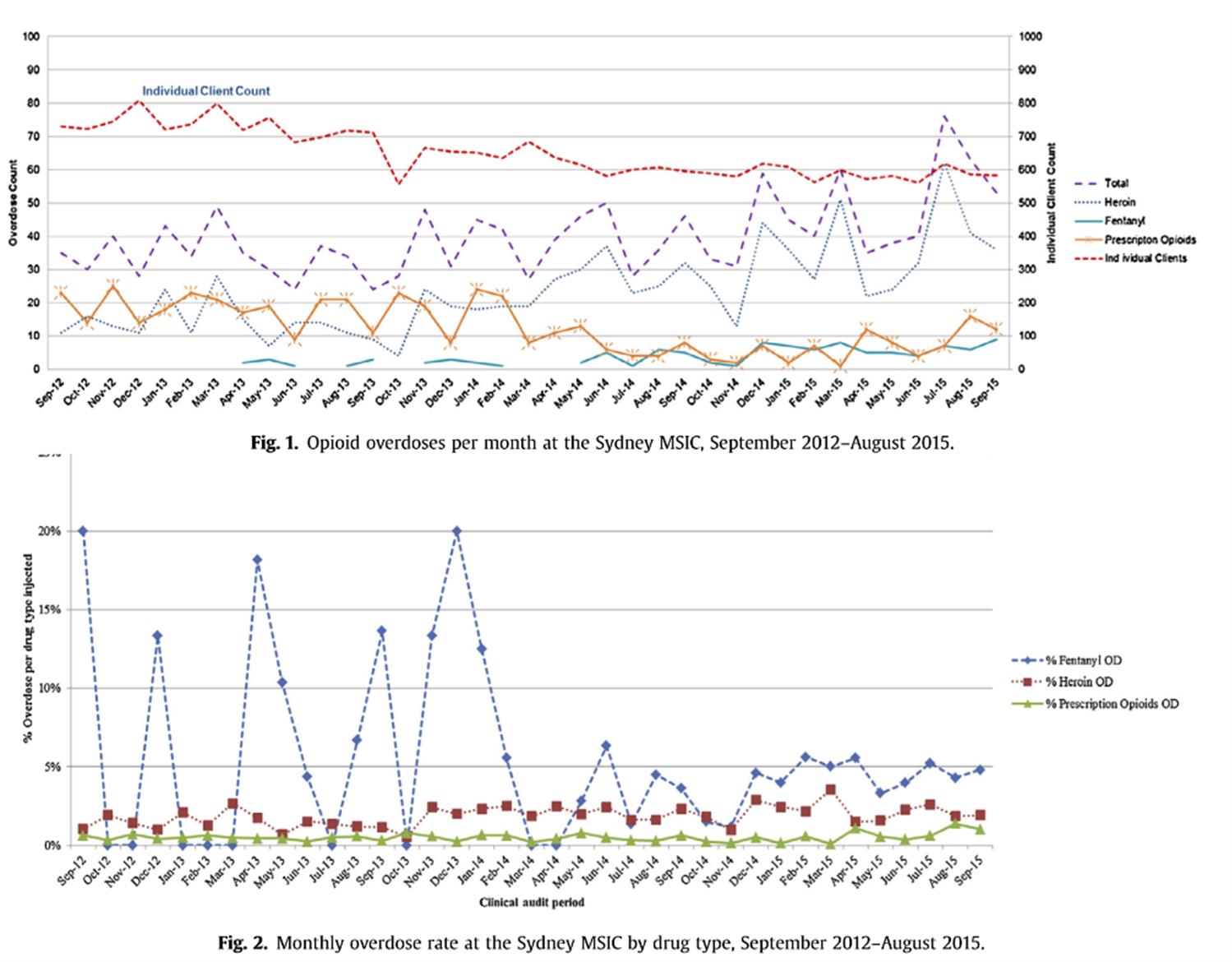
Fentanyl overdose rates at the Sydney Medically Safe Injection Centre 2012-2015. Source: Latimer et al. 2016, p.112-113
The response to the North American public health opioid crisis in Canada has been to promote harm reduction initiatives.
This includes:
The utilisation of peer workforces (people with lived and living experience of drug use), working in collaboration with other mainstream health professionals, to deliver targeted education and (opioid receptor antagonist) naloxone dissemination; fixed-site and pop-up/mobile supervised consumption spaces; drug checking services; and early warning systems. (Canadian Drugs and Substances Strategy’ 2018)
In Australia, the health and harm reduction resources already exist and could be implemented almost immediately to reduce the risks posed by fentanyl and unregulated drug markets more broadly, similar to the Canadian response. But policy barriers limit the ability to offer such services and there seems to be a preference to continue ‘legacy’ systems that prioritise policing the drug market over health-orientated innovation.
Measures that individuals can opt for to reduce some fentanyl-related risks include the use of fentanyl testing strips, peer education, and dissemination of naloxone. Research from McGowan et al. questioned whether the promotion of self-testing strips could be an effective method to detect fentanyl The research concluded that not enough was known at the time of publishing to promote the efficacy of this option and that the major limitation of the test strips was that they do not give any indication to the amount of fentanyl (McGowan et al. 2018). However, another conclusion was that the safest practice for people who use drugs is to do so in the presence of someone with naloxone (McGowan et al. 2018). AIVL member organisations offer education and give out naloxone and a National take-home naloxone roll-out is currently underway.
The Australian Injecting and Illicit Drug Users League (AIVL) recognises the thousands of hospital admissions annually to a drug overdose. Opioid drugs such as fentanyl are the leading cause of drug-induced death in Australia. Peer-based organisations like AIVL have been essential in reducing drug-related harm for decades in Australia.
AIVL’s ‘Spotlight on Overdose’ Campaign recognises that drug overdose doesn’t discriminate, it affects all parts of our community and all walks of society. AIVL calls on governments to recognise the legacy that peer-based organisations have in the prevention and reduction of overdose and to understand that drug overdose is a mainstream issue, the lives of people who use drugs are equally as valuable, and more must be done to prevent deaths and associated harms from an overdose.
Let’s shine a spotlight on overdose and recognise that harm minimisation saves lives.
Article by - Adrian Gorringe (Project Officer - AIVL)
References:
Australian Institute of Health and Welfare 2016, National Drug Strategy Household Survey 2016 Detailed Findings viewed 18 April 2019 https://www.aihw.gov.au/getmedia/15db8c15-7062-4cde-bfa4-3c2079f30af3/21028a.pdf.aspx?inline=true
Australian Institute of Health and Welfare 2018, Alcohol, tobacco & other drugs in Australia: Web report viewed 18 April 2019 https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/drug-types/non-medical-use-of-pharmaceutical-drugs
Gossop, M 2013, Living With Drugs: Seventh Edition, Ashgate Publishing Company, Burlington, U.S.A.
Government of Canada, ‘Harm Reduction: Canadian Drugs and Substances Strategy (2018) <https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/harm-reduction.html>; Laing M. K., Tupper K. W., Fairbairn N. (Dec 2018) ‘Drug checking as a potential strategic overdose response in the fentanyl era.’ Int J Drug Policy, 62:59-66.
Kuczyńska, K, Grzonkowski, P , Kacprzak, Ł & Zawilska, J.B. 2018, ‘Abuse of fentanyl: An emerging problem to face’, Forensic Science International vol.289 p.207-214
McGowen, C, Harris, M, Platt, L, Hope, V & Rhodes, T 2018, ‘Fentanyl self-testing outside supervised injection settings to prevent opioid overdose: Do we know enough to promote it?’, International Journal of Drug Policy vol.58 p.31-36
Mosby, 2013, Mosby’s Medical Dictionary 9th Edition, Mosby Elsevier, St. Louis, U.S.A.
Moss, D, Brown, D & Douglas, BJ 2017, ‘An acetyl fentanyl death in Western Australia’, Australian Journal of Forensic Sciences vol.51 no.1 p.73-77
Quintana, P , Ventrua, M , Grifell, M, Palma, A, Galindo, L , Fornís, I , Gil, C , Carbón, X, Caudevilla, F , Farré, M & Torrens, M 2016 ‘The hidden web and the fentanyl problem: Detection of ocfentanil as an adulterant in heroin’, International Journal of Drug Policy vol.40 p.78-83
Ritter, A; King, T and Lee, N 2017, Drug Use In Australian Society: Second Edition, Oxford University Press, Melbourne, Australia
Rodda, L, Pilgrim, J, Di Rago, M, Crump, K, Gerostamoulos, D & Drummer, O 2017, ‘A Cluster of Fentanyl-Laced Heroin Deaths in 2015 in Melbourne, Australia’, Journal of Analytical Toxicology vol.41 p.318-324
Roxburgh, A , Burns, L , Drummer, O , Pilgrim, J , Farrell, M & Degenhardt, L 2013, ‘Trends in fentanyl prescriptions and fentanyl-related mortality in Australia’, Drug and Alcohol Review vol.32 p.269-275
Stanley, T 2005, ‘Fentanyl: Proceedings of the Symposium “Updates of the Clinical Pharmacology of Opioids with Special Attention to Long-Acting Drugs” Journal of Pain and Symptom Management vol.29 no.55 p.67-71
AIVL is the national organisation representing people who use/have used illicit drugs and is the peak body for the state and territory peer-based drug user organisations.
MEDIA CONTACTS:
Jake Docker, CEO, AIVL – email ceo@aivl.org.au